Immunotherapy and the Head, Neck and Oral Cavity
What it is:
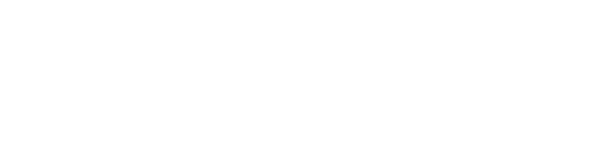
Immunotherapy is a class of medications used to treat cancer by altering an individual’s own immune system. They can act by inducing and enhancing the immune response. Such medicines are now used to treat human cancers, providing an additional approach to control disease.
What it isn’t:
Unlike standard chemotherapies and radiation therapy that can affect both tumor cells as well as the body’s normal cells, immunotherapies directly interacts with the host’s immune system in order to enhance the personal fight against the cancer. The goal of this approach is to utilize the body’s natural defense system to eradicate disease, while trying to minimize side effects.
 There are a number of different types of immunotherapies. The immune checkpoint inhibitors are a prominent class of immunotherapies and represent a breakthrough in cancer care. These medications act through the programmed cell death receptor by blocking the immune checkpoints. Normal cells have ligands that binds to the cell death receptor to allow the immune response know that it is not harmful to the body. In most cancer cells, it produces an abundant amount of ligand that also will bind to the cell death receptor of the T-cells. The ligand is a protein that suppressed the immune response and therefore, allows the mutated cell to evade the body’s immune system from destroying it and grow rapidly into a tumor. Examples include antibodies against (programed cell death protein 1 pathway) PD-1 and the ligand PD-L1 (ex: nivolumab, pembrolizumab).
There are a number of different types of immunotherapies. The immune checkpoint inhibitors are a prominent class of immunotherapies and represent a breakthrough in cancer care. These medications act through the programmed cell death receptor by blocking the immune checkpoints. Normal cells have ligands that binds to the cell death receptor to allow the immune response know that it is not harmful to the body. In most cancer cells, it produces an abundant amount of ligand that also will bind to the cell death receptor of the T-cells. The ligand is a protein that suppressed the immune response and therefore, allows the mutated cell to evade the body’s immune system from destroying it and grow rapidly into a tumor. Examples include antibodies against (programed cell death protein 1 pathway) PD-1 and the ligand PD-L1 (ex: nivolumab, pembrolizumab).
Antibodies to the cytotoxic T-lymphocyte associated antigen-4 (CTLA-4) are another type of immunotherapy and to date these agents have shown remarkable impact upon malignant melanoma. CTLA-4 downregulates the activated T-cells and when they are blocked by antibodies, the T-cell remains active, allowing it to attack the tumor cell. CTLA-4 is currently approved for treatment of melanoma and non-small-cell lung cancer. Both antibody types have similar function to regulate the T-cell activity but contrasts based on its location, variation of expression, timing and etc. A recent trial showed impact in head and neck cancer and these agents are under continuing study in multiple other cancer types, as single therapies, combination immunotherapies and combined with other cancer therapies. It is expected that these medications will become common treatment in many different cancers.
These new therapies are associated with some side effects. While immunotherapy appears to have a good overall benefit-to-risk profile, the most common immune-related side effects are dermatologic and appear to be similar between products. They tend to be mild and manageable with supportive local care, but sometimes more aggressive care might be needed. While these side effects can be troublesome, compare them with those seen in commonly used chemotherapies such as mouth pain (mucositis), dry mouth, taste change, nausea, hair loss, damage to kidney and nerves, and bone marrow suppression.
Risk factors for immunotherapy toxicity are not well characterized but may include increased risk by age, gender, and presence of prior autoimmune conditions. Combined immune therapies increase risk of dermatological side effects and may be associated with increased severity of side effects. Nevertheless, the side effect profile for immunotherapy typically is more favorable than most chemotherapies and/or radiation.
How do you minimize side effects with immunotherapy?
Dose modification, delay in schedule and discontinuing therapy are often considered, but the goal of prevention and management of side effects is to treat the dermatological, oral and other side effects while continuing immunotherapy for the greatest effect upon the cancer. Management may include skin moisturizing and prevention of dehydration, reduced local irritation (avoid tight fitting clothing, wearing light, wicking fabrics), avoiding sun exposure. Washing skin with soap and water can also be helpful. To minimize oral side effects options include good basic oral care, mouth rinses and hydration, avoiding rough abrasive foods, and removal of sharp and potentially irritating dental surfaces.
Dermatologic and oral treatment such as local anti-inflammatory/Immunosuppressive therapy may include steroids (therapy topical/systemic), as well as medications to reduce itching (hydroxyzine, diphenhydramine) and pain. For severe reactions, anti-TNF medications (eg: infliximab) may be considered.
Article contributors include HNCA Board Members: Joel Epstein, M.D., Michael Moore, M.D., Erza Cohen, M.D., and Cherie-Ann Nathan, M.D.
The article is the first in a series on Immunotherapy Treatments.