Ed King
Husband, Father & Partner in a company developing infectious disease diagnostics including a Head and Neck Cancer rapid test; Stage 4 Tongue and Neck Cancer, HPV Negative; Windsor, CO

In August 2014, Ed was diagnosed with squamous cell tongue cancer. Earlier in the month, he noticed a bump on the tip of his tongue that didn’t go away. Cancer was totally unsuspected, either by his family physician or his initial ENT. However, the lab test told a different story.
Ed and his wife quickly discussed what to do and contacted an ENT Surgeon who works with cancer patients, and he recommended a PET scan. The scan not only showed the cancer on the tip of his tongue, but several locations in his neck.
With that information, he proceeded to have tongue surgery, and the ENT was able to get clear margins; however, after discussions locally, and listening to the experience of a local medical doctor who had gone through head and neck cancer, Ed decided to seek treatment at the University Of Colorado Anschutz Cancer Center. From there he proceeded through the next several phases, working with the team that consisting of an ENT surgeon, an oncologist and a radiologist.

The plan was to immediately operate to remove the affected lymph nodes, and to begin daily radiation therapy after a short healing process. Ed’s schedule included weekly infusions and regular visits with a speech therapist and nutritionist. This treatment lasted two months.

The weekly infusions he received were with a medication that is a monoclonal antibody that is supposed to enhance the effects of radiation. Its side effects are unique in that an upper-body rash may develop, and nightly cuts appear on your hands, which, according to Ed, “feel and look like small razor cuts. It is if someone is sneaking in during the night and taking a razor to your fingers.”
Based on the earlier advice he received from the doctor/survivor, who became his mentor during all of this, Ed requested a feeding tube be inserted, and thereby avoided the problems of malnutrition and dehydration. He did manage to eat food along with his liquid diet, but as the treatments progressed, he ate more and more blended foods.
At a Christmas party, he treated himself to blended pork chops, so “he could join the rest of the guests at the dinner table.” He lost about 30 pounds even with the supplemented diet. Thanks to a number of wonderful friends, who transported him back-and-forth to the hospital, a round-trip of about 140 miles each day, he was able to recuperate at home.
The immediate impacts of the treatments included weight loss, very low energy, temporary neuropathy up and down his neck and chest, complete numbness of his neck and lower lip due to the nerve and muscle damage, and his skin became very sensitive to air movements. Even as Spring and Summer approached, he consciously kept his skin covered. This sensation is now gone, but he is still sensitive to cold.
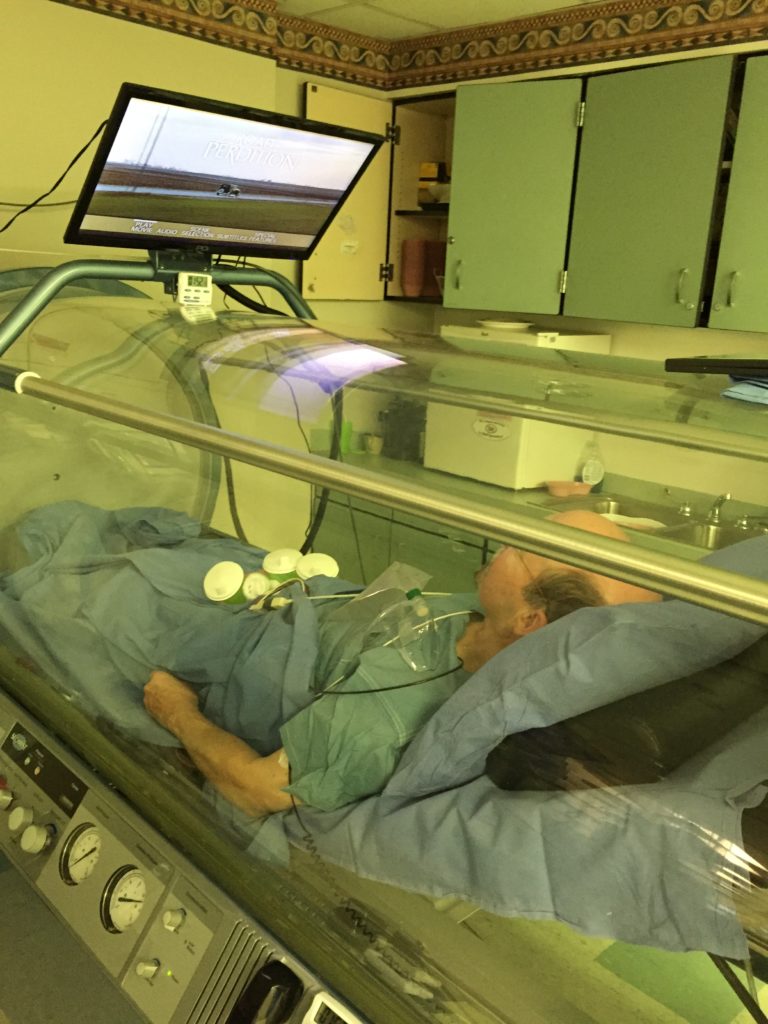
The radiation caused bone necrosis in his left lower jaw. Due to the risk of cancer cells still being present, the ultimate treatment in the hyperbaric chamber was delayed for a year. As all of Ed’s follow-up tests continued to be clear, he underwent a procedure to have several pieces of bone extracted from his lower left jaw, and he spent 3 to 4 hours a day for 40 days in the hyperbaric chamber. This did stop the bone loss. This proved to be a unique event in his life as Ed had been an active SCUBA Diver and one of the primary rules is to practice safe diving and avoid being sent to the hyperbaric chamber.
Because of the earlier mentoring that he had received, and the cancer patients he meets locally in Northern Colorado, Ed decided to start a Head and Neck Cancer support group, and the group has been meeting now for almost five years on a monthly basis.
“We have managed to not only help one another, but to arrange for speakers from all over the United States to join us through video conferencing,” explained Ed. “The members of our group consist of both men and women who were treated many years ago, and new patients who are being treated at various locations both in northern Colorado and outside the state. The video conferencing also allows our out-of-state members to join us.”
Most recently, Ed qualified for a Phase One salivary gland regeneration study at the National Institutes of Health. Most head and neck cancer patients suffer some damage to their salivary glands, ranging from modest impairment to extremely severe impairment. This study may also beneficially impact women with Sjogren’s Syndrome.
Recently, Ed has been named to the statewide University of Colorado Cancer Center Community Advisory Council.
To request Ed for your local event, please contact us at info@headandneck.org or complete the online form.